Traumatic Brachial Plexus Injury
About this PSP
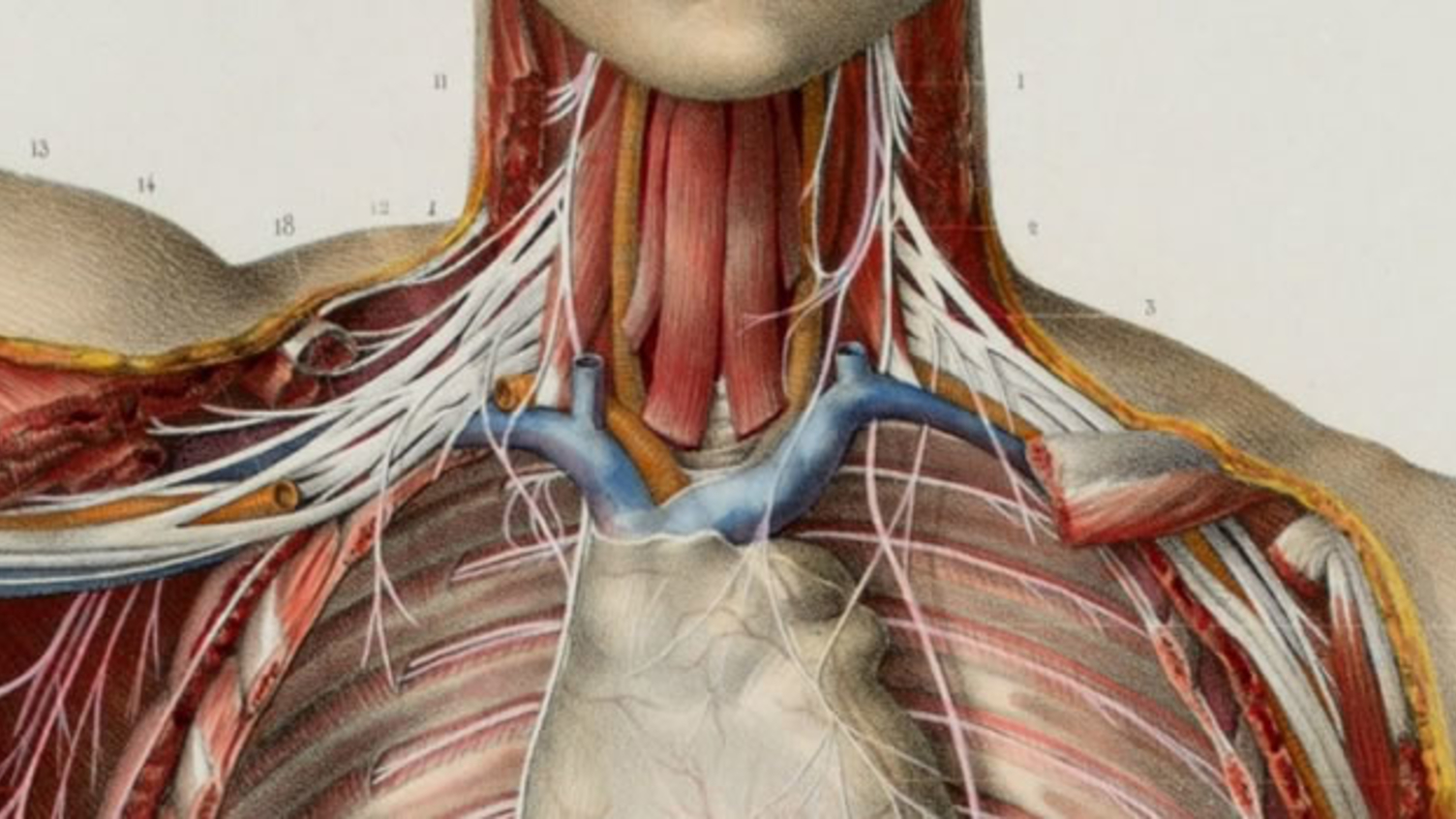
Traumatic Brachial Plexus Injuries (TBPI) are life changing and can lead to permanent changes in function of the arm and hand. The severity of symptoms can vary greatly from person to person, and between different affected nerves and joints. Symptoms can be short-term, lasting a few months, whereas others can experience continuous and severe problems for the rest of their lives. Symptoms can include pain, numbness, stiffness, muscle weakness and reduced movement in the arm and hand.
The PSP is being led by University College London and Royal National Orthopaedic Hospital.
The Traumatic Brachial Plexus Injury PSP Top 10 was published in October 2024.
Top 10 priorities
The most important questions
- Do psychological treatments improve outcomes (e.g. pain, engagement with treatments, acceptance, coping, anxiety, depression, function, PTSD) for people with TBPI. When should they be given and by what methods?
- What is the ideal care pathway for TBPI (from initial injury onwards)?
- What are the best occupational and physiotherapy treatment and management strategies (including hand therapy, exercises, hydrotherapy, massage, electrotherapy, scar management techniques etc.) for TBPI?
- Which tests (i.e. imaging, nerve tests, blood studies, and biomarkers) are able to tell us which patients’ surgery may help?
- How can the results from surgery be better compared to identify: the best time after injury to operate, the best surgical techniques, how well the surgery has worked, and the common risks and complications?
- What are the best ways to promote nerve recovery and healing?
- What are the best pain medications, how often should they be reviewed, which have the least long-term side effects, can new therapies be developed?
- How can muscle fatigue, atrophy and function/control be improved following TBPI?
- How can we (better) support patients who have gone through life changing injuries?
- What robotic technology or devices can better assist and support arm and hand function in someone with a TBPI?
The following questions were also discussed and put in order of priority at the workshop:
- How can we predict how long will it take to recover, and how good the recovery will be, and can this be improved?
- What is the impact of TBPI on friends and family and how can they be supported?
- What is the best treatment for total brachial plexus injuries (complete arm paralysis)?
- How can we better predict outcomes by using nerve tests or measurements during surgery?
- Which technique(s) can accurately and reliably diagnose a nerve root avulsion (nerves pulled out from spinal cord) and once diagnosed how are these best treated?
- What functional outcomes are considered when making decisions about surgery?
- What alternative medicines and supplements (including CBD, medical marijuana, vitamins, animal venoms and compounds) are effective in treating TBPI and its associated nerve pain?
- What are the long-term effects on the body (e.g. musculoskeletal system, cardiovascular system, skin, other organs, and systems) in a person with TBPI?
- Would a national database or registry aid monitoring of patient recovery?
- Does early assessment, diagnosis and treatment improve the chance of normal function?
- Does the use of a standardised method of assessment improve treatment and outcomes for people with a TBPI?
Key documents
These documents set out the aims, objectives and commitments of the PSP.
Traumatic Brachial Plexus Injury PSP protocol
Traumatic Brachial Plexus Injury PSP Steering Group terms of reference