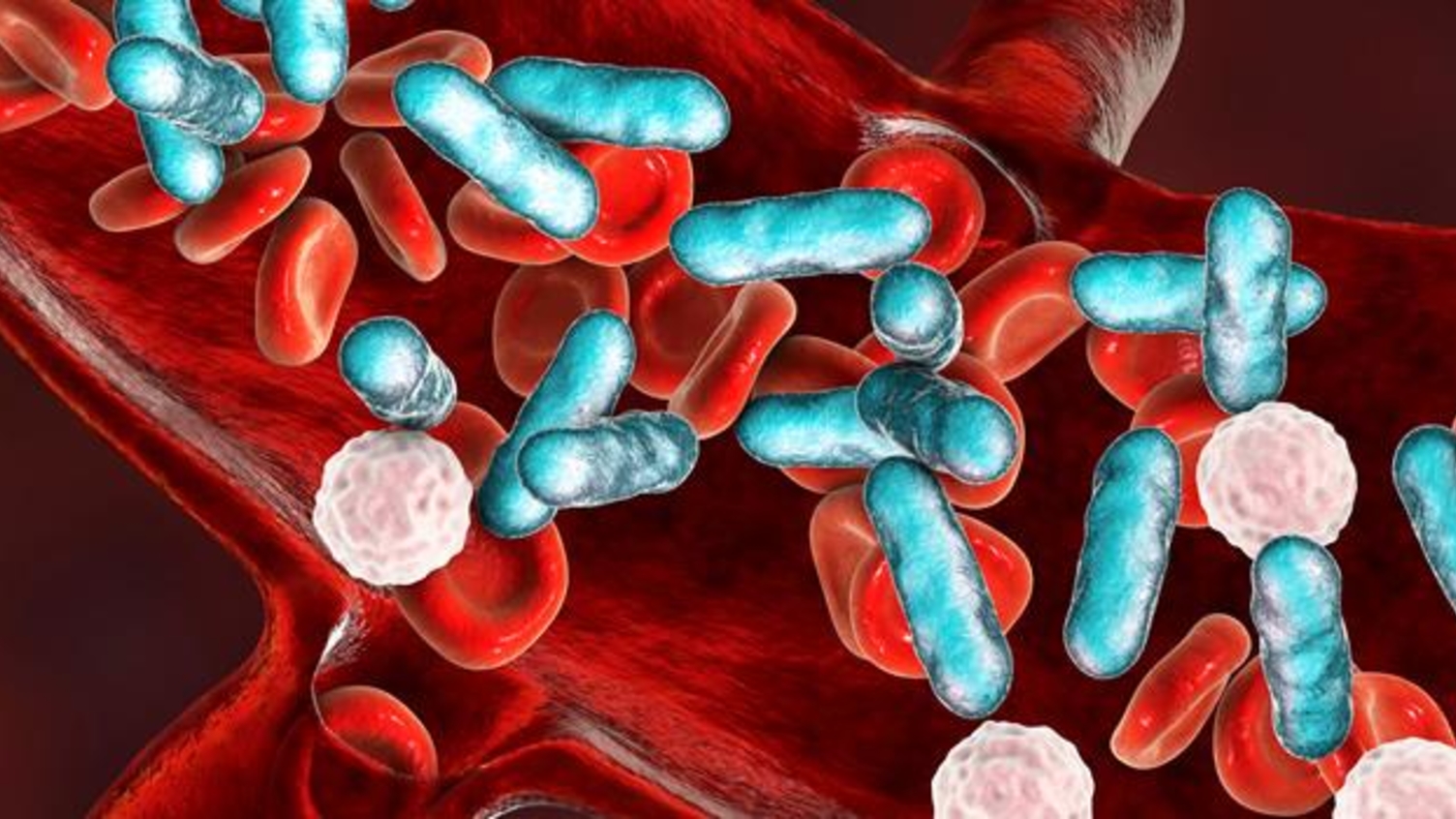
Sepsis
About this Priority Setting Partnership
The goal of the PSP was to understand the mechanisms of sepsis better and to improve diagnosis, treatment and patient outcomes.
Sepsis is a life-threatening condition where the body overreacts in response to an infection.
The PSP was funded by Sepsis Research FEAT.
The Sepsis PSP Top 10 was published in September 2024.
In this video, PSP Steering Group members explain the Sepsis PSP.
More information
Top 10 priorities
The most important questions
- How can the diagnosis of sepsis become faster, more accurate and reliable?
- What are the long-term effects on the body from sepsis (sometimes called post-sepsis syndrome)? How are these long-term effects best treated and managed?
- What is the role of treatments other than antibiotics in the care and management of sepsis?
- Can diagnostic tests be developed for sepsis that can be used wherever the person is receiving care (e.g. in a GP surgery, hospital, ambulance or at home)?
- Why and how do some people with sepsis become seriously ill very quickly?
- Would specialist sepsis services improve outcomes for people with sepsis during hospital treatment and for follow-up care?
- Are there ways to tailor treatment of sepsis to the individual (e.g. based on blood markers or other indicators)?
- How does an infection lead to sepsis?
- Would treatment before admission to hospital (e.g. provided by GPs or ambulance crews) improve outcomes for people with sepsis?
- What are the safest and most effective ways to treat sepsis using antibiotics?
The following questions were also discussed and put in order of priority at the workshop:
- Are there ways to prevent long-term effects on the body (sometimes called post-sepsis syndrome) through treatment while the person has sepsis?
- What are the barriers to people with sepsis receiving rapid treatment once diagnosed, and how can these be overcome?
- What factors (e.g. genetics, age or ethnic background) influence whether a person recovers or dies from sepsis, and how well a person recovers?
- What happens during sepsis to cause long-term effects on the body (sometimes called post-sepsis syndrome)?
- How often is sepsis genuinely missed? Why does this happen? What would help health professionals to recognise sepsis (e.g. additional training)?
- How can communication and care co-ordination be improved across the teams of health professionals caring for people with sepsis?
- Are there any aspects of intensive care/ hospital treatments that increase the risk of becoming seriously ill with sepsis?
- What impact is Sepsis Six (a set of six steps to be taken within an hour of sepsis diagnosis) having on the recognition and treatment of sepsis?
- Does sepsis affect the immune system in the long term, increasing the risk of infections and/or autoimmune conditions? If yes, how is this best treated and managed?
- Can a test be developed to predict the outcome of sepsis, to identify which people are likely to recover, or become seriously ill or die?
- Does living in poverty increase the risk of developing sepsis and/or lead to worse outcomes? If yes, how and why does this happen?
- What are the best ways to monitor people after sepsis and to provide follow-up care?
- How likely are people to experience repeat episodes of sepsis? Are repeat episodes different to the first experience?
- Does sepsis increase the risk of developing long-term conditions (e.g. heart disease and chronic kidney disease)? How are these conditions best treated?
- Are some people at greater risk of developing sepsis because of their genetic make-up? Does this mean their family members are also at risk?
Key documents
These documents set out the aims, objectives and commitments of the PSP.
Sepsis PSP Steering Group terms of reference